Introduction: Central nervous system (CNS) relapse is a relatively infrequent but often fatal complication of the most common subtype of non-Hodgkin lymphoma, diffuse large B-cell lymphoma (DLBCL). Median overall survival (OS) after DLBCL relapse in the CNS is about 4 months. Despite identifying patients at high risk of developing CNS relapse using the CNS international prognostic index (CNS-IPI) score, it has been difficult to validate any specific strategy. Various chemotherapies and administration methods have been tested. Thus far, only the addition of rituximab to chemotherapy has yielded significant results. Our objective is to determine if administering prophylactic chemotherapy is efficacious in preventing DLBCL relapse in the CNS.
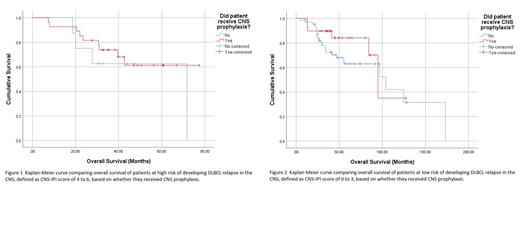
Methodology: We collected retrospective data for patients with newly diagnosed DLBCL treated with rituximab and anthracycline-based chemotherapy from 2010 to 2020 in the Northwell Health system to determine the efficacy of CNS prophylaxis. Patients with CNS disease at diagnosis, primary testicular lymphoma, primary mediastinal large B-cell lymphoma, and HIV-associated lymphoma were excluded from this study. CNS prophylaxis was defined as receiving at least two doses of prophylactic chemotherapy, whether intravenous or intrathecal. Follow up for at least one year after diagnosis was required for inclusion. Overall survival (OS) was defined as the time difference between the date of definitive diagnosis to death or last date of contact. Other potential prognostic factors including double hit status and cell of origin, germinal center B-cell (GCB) vs. non-germinal center B-cell (non-GCB), were also evaluated. Pearson's chi-square analysis was used to compare the rate of DLBCL relapse in the CNS based on whether patients received CNS prophylaxis. Low risk was defined as CNS-IPI score 0 to 3 and high risk as CNS-IPI score 4 to 6. Kaplan-Meier analysis with log-rank (Mantel-Cox) testing was used to determine if any significant OS benefit was observed for the low and high-risk groups based on CNS-IPI score.
Results: Of the 437 charts reviewed, 127 were eligible for inclusion. Most patients were male (56.7%). Median age was 69 years and median Eastern Cooperative Oncology Group (ECOG) performance status was 1. Most cases were non-GCB (44.9%, as 25% of cases were missing data) and not double hit (85%). Of the 35 patients at high risk for CNS relapse, 27 (77%) received prophylaxis. Intrathecal methotrexate (IT MTX) was given to 26 patients (96%) and high dose intravenous methotrexate (HD MTX) was given to 1 patient. CNS relapse occurred in 6 patients, of which 5 had a low-risk CNS-IPI score. One of the five patients in the low-risk group and the one patient in the high-risk group that had CNS relapse received prophylaxis. No significant difference in overall relapse rates were observed based on whether prophylaxis was given, X 2 (1, N = 127) = 0.30, p = .59. Kaplan-Meier analysis showed no difference in OS after stratification of patients by CNS-IPI score into the high-risk ( p = .50) and low-risk ( p = .24) groups. HD MTX was not administered frequently enough to determine its efficacy. Neither cell of origin (X 2 (1, N = 95) = 2.95, p = .086) nor double hit status (X 2 (1, N = 127) = 1.512, p = .22) had any significant effect on OS.
Conclusions: We did not observe any clear benefit for administering IT MTX to prevent DLBCL relapse in the CNS. Most of the CNS relapse events occurred in the low-risk group, even though 8 patients in the high-risk group did not receive any CNS prophylaxis. This study did not have sufficient power to make a definitive conclusion. As CNS relapse is a rare event, a much larger sample size is required to determine the true efficacy of CNS prophylaxis. Non-GCB cell origin and positive double hit status are not included in the CNS-IPI score but their potential association with risk of DLBCL relapse in the CNS is understudied. Future studies should build upon these findings.
Disclosures
No relevant conflicts of interest to declare.